Forum
In 2011, IAEN held an online discussion forum on efficiency and effectiveness in the context of HIV and AIDS. Experts from a variety of organizations and disciplines posted short discussion pieces on various aspects of this topic. This forum was designed to encourage online discussion among members. Inclusion of documents or posting of comments does not imply endorsement by IAEN or sponsoring organizations.
Introduction to the IAEN forum
April 28, 2011
I would like to formally welcome you to the International AIDS and Economics Network. IAEN has been in existence for over 17 years, yet we continue to evolve as an organization. When this organization began, it represented the only forum in which "AIDS economists" in Washington DC could meet and discuss issues such as the macroeconomic impact of AIDS, AIDS and its impact on agriculture and the workplace, the cost and cost-effectiveness of HIV/AIDS programs, etc.
Over time IAEN has managed to expand its scope, both in terms of reaching individuals globally as well as expanding its focus beyond the small number of economists who work exclusively in the field of HIV/AIDS. IAEN members are not only researchers in the field of AIDS and economics, but also policymakers and other decisionmakers who are ultimately the consumers of information which gets collected on the issue of AIDS and economics. IAEN has also expanded beyond being just an organization with "face-to-face meetings", by utilizing virtual social media (e.g., Linkedin) to encourage the dissemination of the latest research as well as encouraging discussions on topics of critical interest.
As a member of the IAEN, we would ask for your participation in a number of ways. First, we ask that you take the chance in your busy schedules to read the relevant documents which we place online, both on the IAEN Linkedin group and as part of the IAEN website (www.iaen.org). Second, we would ask that you provide feedback and comments on these articles. Finally, we would ask you to identify articles that you believe would be of interest to other members of the IAEN and to share these whenever possible.
Introduction to the IAEN Forum on Effectiveness and Efficiency
The next step in the evolution of the IAEN is this forum, a discussion among economists and policymakers on the topic of efficiency and effectiveness of HIV/AIDS resources. The IAEN has requested that a number of researchers write short (generally no less than 1 page) thought pieces on the topic of HIV and AIDS. These will then serve as a starting point for our discussions on this topic.
The topic for this forum, "efficiency and effectiveness of HIV/AIDS interventions" was selected for a number of reasons. While this has been an issue of concern for economists for many years, it has not been a topic which was on the top of the agenda for donors throughout most of the last decade. Not surprisingly, effectiveness and efficiency has become a bigger and more critical issue as resources stopped growing throughout the last three years. By all indications, the current period of "flat line funding", especially by PEPFAR and the Global Fund, will become a regular and long-term part of our vocabulary. While in the past it was necessary to adjust to the reality of rapid growth, we now face the very real situation of long-term stagnant funding. How should we, as economists and policymakers, respond to this new reality?
When discussing "value for money" (which IÆll used interchangeably with "effectiveness and efficiency") in regards to HIV and AIDS, I tend to focus on 3 issues: 1) How much money do we need (cost), 2) Are we allocating it in a way to achieve the greatest possible impact (effectiveness) and 3) Are we truly spending our resources so that we achieve the best quality output for the resources we are spending (efficiency)?
How Much Money Do We Need?
Do we have enough money? By most accounts, we must conclude: 1) the level of resources available for prevention and treatment has increased dramatically in the last decade (reaching $15.9 billion in 2009), and 2) these resources remain inadequate to assure that the goal of universal access is achieved (UNAIDS estimates that over $25 billion was required in 2010). Even more worrying, data indicate that the level of international resources spent on HIV and AIDS declined for the first time ever in 2009.
When UNGASS was first being launched, economists projected that funding would need to increase to about $10 billion by 2005, an increase of nearly 10 fold from existing levels. As someone involved in those early predictions, I was very pessimistic about the feasibility of achieving such an optimistic goal in generating new resources. However, new spending (especially from the US government under the auspices of PEPFAR and from the global community under the Global Fund) did increase dramatically, reaching $8.3 billionby 2005. Yet the good news about resource generation was tempered by the fact that many of the other UNGASS targets were not achieved.
One of the challenges economists and policymakers face in terms of estimating resource needs is that despite over 30 years of progress, we still donÆt have a solid understanding of what interventions should really cost. Some of the most comprehensive data collection on costs from PANCEA indicated that unit costs were wildly different, not only across countries but also within them. Meanwhile research on the costs of orphan programs indicate further wild variations, ranging from as low as $63 in Ethiopia and as high as $946 in Botswana. This raises the question of how donors should be budgeting their increasingly limited resources? What does it really cost to effectively and efficiently reach an orphan with at least a minimum package of useful services?
The reality of "flat line funding" has perhaps most dramatically affected countries which had the greatest initial success in moving towards universal access. Latin America, for example, rapidly expanded ARV coverage, reaching 49% by 2008. However, by 2009, coverage had only inched up by an additional 2%. Similarly in North Africa and the Middle East, ARV coverage only increased from 10% in 2008 to 11% in 2009.
Are We Allocating Available Funds Wisely?
Given an environment of severely constrained resources, one solution is to reallocate funds in order to assure that the greatest possible impact is achieved.
"The resource availability for the AIDS response has always fallen short of what is needed. National programmes have had to ensure that programme choices are effective and efficient to have the maximum impact in averting new HIV infections and AIDS-related deaths. Countries have seen best results when resources are tailored to epidemic patterns and have followed evidence: for example, treatment programmes that use the most effective combination of drugs and male circumcision as a priority component of prevention in generalized epidemics. In many countries, programmes promoting abstinence received far more resources than efforts to increase condom use or reduce multiple partners. Evidence from Zambia shows that, without the right mix of behavioural interventions, gains are minimal." - UNAIDS. "Global Report 2010".
The issue of allocative efficiency has been discussed widely in a number of publications, with numerous and disturbing examples of HIV prevention resources being allocated to interventions which are unlikely to have an impact on the epidemic. The most striking examples include cases of resources being focused on the general population when the epidemic is actually spreading among most-at-risk populations (MARPs).
There is a need to determine what is the optimal allocation of resources for any one country. The nature of the epidemic in any country, as well as issues of cost and culture, should all play a role in determining what is optimal allocation of HIV and AIDS resources. However, at this point in time, insufficient economic or epidemiologic research is available to guide countries in their determination of the optimal allocation of funds.
Are We Using Funds Efficiently?
In addition to allocative efficiency, we should also consider whether funds are actually being used in the most efficient way possible. Male circumcision presents a particularly interesting example of how important efficiency can be. In this case, task sharing and task shifting have been shown to be essential in any roll-out of MC services.
Efficiency also requires that we have a clear understanding of which services within an intervention are actually going to improve the quality of life of the clients receiving these services. Programs designed to reach orphans and vulnerable children (OVC) have consumed a significant quantity of all HIV and AIDS resources, yet little is known about which OVC interventions actually increase the quality of life of the children being reached. Should OVC programs, for example, focus more on food and nutrition, legal rights, shelter, income-generating activities, education, etc? How effective is the delivery of these services? Sadly there are significant gaps in our understanding about what is meant by "efficient OVC programs".
Conclusion
Throughout this forum, I hope that we will make progress in better understanding how much is required, how those resources should be allocated and how we may be better placed to efficiently spend those resources which are available.
Steven Forsythe
IAEN President
Country Ownership, But of What? The Case for Efficiency and Effectiveness
May 5, 2011
Arin Dutta PhD and Farley Cleghorn MD, MPH
Futures Group
The global public health community has been actively engaged in debating and strategizing the concept of country ownership; it is finally the moment for putting words into action. There are several frameworks and initiatives ongoing in this context, from the Paris Declaration to the Three Ones and we will pick one to make our point.
A McKinsey initiative on country ownership, funded separately by the US government and the Gates Foundation, is to begin in South Africa and Botswana by engaging government, international technical agencies and implementing partners. This initiative aims to produce a working understanding of how to implement and measure country ownership. We discuss this initiative and use it as a case for including efficiency and effectiveness—doing more with less—as an objective in implementing country ownership, and as an indicator of the success of country ownership for HIV/AIDS programs.
The McKinsey initiative has identified four draft country ownership criteria to further the common understanding of all partners. Later we will also use these as a framework for discussing efficiency and effectiveness. The criteria are rendered with country and donor perspectives:
(1) Political ownership/stewardship: from a country perspective, this codifies and makes visible the government's role as architect and overseer of the overall process with input from other sectors. From a donor perspective, country ownership is held as a core principle by all agencies and takes priority in aid relations.
(2) Institutional ownership in a country perspective requires local entities (government, NGOs, civil society, private sector) to make decisions, bear responsibility, and manage funds. From a donor perspective, participation is necessary to help shape the process and to help ensure that civil society is supported as a partner.
(3) Capabilities reside in local institutions, as above, who implement, perform or outsource activities. They also refine and modify programs based on evidence at each stage. Donors would in turn align their organization, vision, plan, activities, allocations, and evaluations to the national strategy as well as the idea of country ownership.
(4) Accountability of the local institutions for services and results to citizens as well as donors through performance-linked, transparent mechanisms with measurable outcomes. Civil society would contribute feedback into the mechanism. Between the donor and the country, mutual accountability would obtain, with checks and balances, clear communication of incentives/penalties, responsibilities, and ways to agree and measure outcomes.
The current resource crisis in HIV/AIDS programming is a function of declining or plateauing financing and increasing demands of scale and complexity. Additionally, the focus on disseminating treatment gains has not been matched by prevention success and hence long run costs based on present conditions are not sustainable even in middle income countries. It is the primary motivator for seeking more effective interventions that generate more output for current level of resources and efficiency gains that produce the current level of output for fewer resources. We argue below that efficiency and effectiveness initiatives clearly reflect the attitudes exemplified by the four criteria above, and hence should be one of the primary objectives of country ownership. Indeed, efficiency and effectiveness is the answer to the question: "what should be owned (by countries)"?
First, putting in place efficient and effective HIV/AIDS program management strategies is now a political imperative for national stakeholders. The international financing situation has reached a point of inflexibility where a plateau in PEPFAR-2 contributions has been manifest over the last few years. Recently the Global Fund received firm pledges in its recent replenishment of only 70% of an amount it thinks will finance future activities at "significantly lower levels". Even so, leaders of HIV/AIDS programs have made commitments to PLHIV in their countries to scale-up services of all kinds and to improve quality of care. This contradiction cannot be resolved without a commitment to sustainability that invokes efficiency and effectiveness. And the situation where local stakeholders do not architect and oversee such a process is not tenable. Country government leaders must be visibly willing to own a process which is known to be sustainable or leads to sustainability, and this must be understood and supported by donor partners.
Second, responsibilities for efficiency and effectiveness are rooted in institutional roles. There is no one institution which can deliver on the entire panoply of initiatives that are needed to achieve significant and lasting gains. For example, greater effectiveness in service delivery for HIV treatment will require more effort in learning, improving, and evaluating by government, NGO or for-profit implementers, health workers, etc. Similarly, efficiency gains can be made by better procurement practices or process improvement, both stemming from partnerships that challenge established public-private linkages. Responsibility for sustaining the gains must fall on civil society and donor partners. All of the institutions can own components of the efficiency and effectiveness process. This can be described as meaningful multi-sectoralism.
Third, ownership of the efficiency and effectiveness process is deeply woven with an understanding of capabilities. Technical knowledge to find and enact the necessary change resides in key implementers and technical agencies. The ability to oversee, evaluate, and finance the changes resides with government and donors. Understanding such capability also clarifies roles. Country ownership defined without reference to capacities will very likely not be implemented. An efficiency and effectiveness focus here clarifies capacity to the extent that country ownership begins to move forward and can take on bigger and brighter overtones.
Fourth, the process of achieving efficiency and effectiveness gains can be a marker of accountability for the local stakeholders across the process, and an indicator of their desire to create positive change. Sustainability is the best proof of the government's desire to become a steward of the destiny of the HIV/AIDS sector, and a demonstration of its commitment to the citizens as well as the international partners. Relatedly, supporting this change is the best way such partners can show that they too are willing to be held accountable to the demands of the current resource-constrained era.
Country ownership and the continuous improvement process that is hinted at by efficiency and effectiveness in HIV/AIDS programming are intertwined in our understanding. Not just because sustainability is in such crisis in the sector, but because success in this field will ensure that country ownership becomes an actual, living principle rather than an abstract concept.
Arin Dutta and Farley Cleghorn, Futures Group
Other people's money - would more domestic fiscal effort lead to greater efficiency?
May 12, 2011
Robert Hecht, Results for Development Institute
In the current debate on how to improve effectiveness and efficiency in AIDS programs, especially in low and middle income countries, a lot of excellent thinking and analysis are being done on the technical aspects of this problem. Members of the IAEN are playing an important role in this.
But what about the politics of who pays for an expanded AIDS effort in the coming years? I argue here that this is also having an influence on effectiveness and efficiency, and could become an even more important driver than it is today, if used in the right way.
-----------------------------------
On the technical side, national AIDS experts and their international colleagues are looking carefully, for example, at how to target HIV prevention efforts better at the sub-populations where the most new infections are occurring (aided by the new "modes of transmission" methods) and at the interventions that we know, or feel more confident from recent analysis, are really working. Again, new insights from cost-effectiveness studies and program evaluations are being nicely fed back into policy decisions.
Ditto on the treatment side, where even more energy is going into parsing anti-retroviral therapy program costs and identifying ways to bring down the unit cost of treating AIDS patients commensurate with good quality and health outcomes. The plethora of analysis being conducted by many organizations, including PEPFAR and its collaborators from Boston University, CDC, and MACRO are adding tremendously to our knowledge and ability to identify ways to "make the money go farther" in treatment.
--------------------------------------
At the same time, there is increasing discussion and debate around who will pay for these expanding national AIDS efforts in low and middle income countries, even as these efforts become more efficient (fingers crossed). Governments and donors will be facing an AIDS bill for prevention, treatment, and orphan care in the tens of billions of dollars for years and decades to come, and unfortunately that bill can be expected to grow almost everywhere -- even with efficiency gains — as our own work for the aids2031 project has shown.
We have argued elsewhere that national governments should be paying a larger share of that bill than they are today. Many low income countries have become highly dependent on outside funds to support their national AIDS programs — as much as 90 percent or more in some countries such as Mozambique and Vietnam. This is dangerous for these countries and their HIV positive citizens, especially at a time when donor assistance for AIDS has plateaued and is by its nature unpredictable. It is also inequitable, especially when bilateral and multilateral aid (from the Global Fund, for example) is directed to middle income countries with concentrated epidemics such as China and Mexico. Surely these countries can afford to pay for their own national AIDS efforts.
----------------------------------
But is there another link between increasing national financial (self)reliance for AIDS spending, and greater program efficiency? It may not be farfetched to imagine that national AIDS authorities, officials in national finance ministries, civil society watchdog groups, and others will be more concerned about value-for-money when it is the country´s own hard earned revenues, rather than donor funding. Do national authorities really make hard choices about prevention spending and lowering the cost of ART, when they are basically spending "other people´s money", as they do today?
The connection between "it´s my hard earned money" and "so I´m going to make sure it´s spent well" is far from straightforward and automatic, and no doubt there are examples of domestic funds for AIDS being squandered. But there is some anecdotal evidence to suggest that national authorities take the efficiency and effectiveness issues more seriously when they are spending their own money and not money flowing from Washington or Geneva.
In Cambodia, where donor funding is flattening and the future of outside support for AIDS is seen as highly uncertain, the government has decided to refocus its prevention efforts on most at risk populations, cutting its planned prevention spending by tens of millions of dollars. The link between this decision and a simultaneous move to expand the domestic share of the AIDS budget from 10 percent to 50 percent is certainly not accidental. Just ask the head of the Cambodian AIDS program.
In Thailand, too, where outside financial support has been cut in recent years and now accounts for just 3 percent of the country´s spending, the government is nearly obsessive about enhancing prevention effectiveness and lowering the costs of treatment. Ditto for South Africa, where about three-quarters of AIDS spending of over $2 billion a year is assumed by the government. There is a big push on in South Africa to lowering average treatment costs through better procurement of drugs and tests and less expensive clinic and community-based approaches to initiating and sustaining ART.
---------------------------------
Has the time come to see hard talk in all countries, even the poorest, about who pays for AIDS services as an important part of the "effectiveness and efficiency" agenda?
Efficiency and Effectiveness of HIV/AIDS Policies and Interventions
May 19, 2011
By Ilaria Regondi and Alan Whiteside (HEARD, University of KwaZulu-Natal)
Why focus on efficiency and effectiveness?
Efficiency is one of the key underpinnings of economic theory. Economists argue that the achievement of greater efficiency from scarce resources should be a major criterion for priority setting (Palmer and Torgerson 1999). In the health sector, efficiency measures whether healthcare resources are being used to get the best value for money. In the current context of scarce resources for development, achieving better value for money for HIV/AIDS services, programmes and policies is essential.
What do we mean by efficiency and effectiveness?
Technical efficiency is defined as the ability to produce a given level of output with a minimum quantity of inputs. Allocative efficiency refers to the ability to choose optimum input levels for given factor prices. It takes account not only of the productive efficiency with which healthcare resources are used to produce health outcomes but also the efficiency with which these outcomes are distributed (Palmer and Torgerson 1999). Effectiveness generally refers to the ability of an intervention to achieve its desired outcome. Cost-effectiveness analysis (CEA) is a form of economic analysis that compares the relative costs and outcomes of two or more interventions or courses of action. In relation to HIV/AIDS, cost-effectiveness studies most often evaluate prevention measures on the basis of cost per infection averted, quality or disability adjusted life-years (QALYs, DALYS).
What are some of the key issues relating to the effectiveness and efficiency of the AIDS response?
• There is much room for improvement in the efficiency of the global HIV response, both at an international, national and district/facility level. Today, we have many more tools at our disposal to increase efficiency than we did in the past. We must urgently make these tools available to implementers of HIV services and programmes.
- There is limited evidence available on the cost-effectiveness of key HIV/AIDS services. This is in part due to the difficulty of obtaining accurate epidemiological and cost data.
- There is a trade-off between producing more consistent cost data and doing more sophisticated analyses with the data that we currently have. Greater harmonization of existing and future cost data is necessary across agencies and countries.
• We know that there are large variations in costs between countries and within countries (at the district/facility level). ARVs continue to be major cost drivers, so efforts to collectively drive prices down must persist.
• There is limited evidence to support further scale-up and sustainability of integration of voluntary counselling and testing (VCT) and sexual and reproductive health in a wide variety of settings.
• Performance-based financing shows promise for both treatment and prevention of HIV, but more systematic evidence is necessary.
What do we still need to find out?
More research is needed in the following areas:
- Cost-effectiveness analysis on new WHO guidelines relating to initiation of ARV treatment and on adherence to treatment.
- More systematic analyses (meta-analyses, meta-regressions) to examine facility-level ART costs as well as to explore the effectiveness of risk-factor interventions in reducing HIV/AIDS vulnerability.
- Look beyond the field of HIV/AIDS to learn more about technical efficiency.
- Further explore evidence on performance-based financing. One example would be to use conditional cash transfers to improve ART adherence.
- Exploration of how integration of HIV services impacts effectiveness, what are the best methods of implementation and whether gains can be made at scale.
What we are doing to explore the efficiency and effectiveness of the HIV/AIDS response?
The UNAIDS/World Bank Economics Reference Group (ERG) brings together high-calibre economists and practitioners to provide expert advice and inform policy makers on the latest findings and research trends to inspire evidence-based interventions. Its last meeting took place in Geneva on 7 and 8 March 2011. The meeting discussed the efficiency and effectiveness of AIDS policies and interventions at length. It aims to produce a set of policy recommendations to guide the future programmatic and research direction of the sponsoring bodies.
References:
Palmer, S., Torgerson, D., (24 April 1999). "Definitions of Efficiency." British Medical Journal. 318: 1136. http://www.bmj.com/content/318/7191/1136.full
UNAIDS/World Bank Economics Reference Group: http://www.heard.org.za/research/economics-reference-group/eighth-meeting
What are the most cost-effective HIV/AIDS interventions?
May 26, 2011
John Stover
The cost-effectiveness of HIV interventions varies by epidemic so there is no single answer to this question. To further complicate matters we have relatively good cost and effectiveness information on key biomedical interventions such as ART, male circumcision, condoms and the prevention of mother-to-child transmission (PMTCT). Cost and impact are much harder to define for behavior change interventions such as behavior change communications, community mobilization, and school-based education because there are few standard definitions of what each intervention includes. More information is available for some behavior change interventions such as counseling and testing and outreach to key populations.
Accurate measurement of cost-effectiveness of prevention interventions requires randomized controlled trials to accurately measure impact and cost. But few such studies exist. Instead modeling is often used to estimate cost-effectiveness in certain epidemic settings. At Futures Institute we have developed the Goals model for such calculations and used it to estimate impact and cost-effectiveness for national strategic planning. When we look at the findings from applications across the world, some general conclusions do emerge.
For generalized epidemics male circumcision is very cost-effective in all countries in which current rates of male circumcision are low. PMTCT is generally cost-effective especially at high levels of HIV prevalence. Condoms promotion and outreach to sex workers and clients are also very cost-effective in most settings. Of course, ART is cost-effective in preventing AIDS deaths and can have a significant prevention impact as well.
For concentrated epidemics the picture is more varied depending on the main drivers of the epidemic. In those epidemics driven by transmission among injecting drug users, outreach to IDU and needle and syringe exchange programs are very cost-effective. Outreach to sex workers and clients, outreach to men who have sex with men, and condom promotion are also generally cost-effective prevention interventions. ART is cost-effective at preventing death.
UNAIDS has recently defined a set of "basic programs" that have demonstrated effectiveness and should be scaled-up in all countries. The set includes PMTCT; condom promotion and distribution; outreach to key populations (sex work, IDU, MSM); treatment, care and support for people living with HIV; male circumcision in generalized epidemics with low male circumcision rates; and social and behavioral change communications.
Other interventions may be cost-effective in specific settings but not in others.
Fighting a Concentrated Epidemic: MARPs in Vietnam
June 2, 2011
William McGreevey
Department of International Health, Georgetown University
Vietnam has a concentrated epidemic focused in injecting drug users (IDU), more than a quarter of whom are HIV+, and other most-at-risk populations (MARPs) including sex workers, where HIV prevalence is just under five percent. There is significant crossover of risk behavior, for example, rising trends in drug use behavior among sex workers. The most recent Government of Viet Nam report to UNGASS notes that the epidemic may have begun to stabilize in many locations among these populations but is rising in others such as in the northwest (Dien Bien and Son La). In 2009 national adult HIV prevalence was (aged 15-49) was 0.43 percent. HIV prevalence tends to be positively correlated with population density, which will increase substantially in Vietnam, with an estimated 43 percent of its population in the urban areas by 2030.
Over the past 10 years Viet Nam has strengthened the policy and legal environment governing HIV. Significant developments include the National Strategy on HIV/AIDS Prevention and Control (2004-2010) and the Law on HIV/AIDS Prevention and Control passed in 2006. Other more recent innovations include the amendment to the law on drug control which permits the use of harm reduction. While there have been significant advances in programs and interventions for MARPS groups, policy and legal gaps and tensions remain. Under the 2003 Ordinance on Prostitution Prevention and Control, anyone selling sex is subject to administrative detention; similarly the Ordinance on Administrative Violations and Decree 94 of the new law on drugs contain provisions to detain drug users in compulsory settings and limit access to HIV and harm reduction services.[1] How and in what measure do interventions focused on most-at-risk populations yield benefits adequate to repay program costs?
Lives saved and future care and treatment averted by keeping IDU, sex workers and MSM free of HIV can add up to benefits that substantially exceed program costs over coming years. The value of lives saved can be estimated using methods developed and tested by respected health economists in the USA and other countries. Likely and ?Çÿcounterfactual´ scenarios can identify cost savings as well as life enhancement results. Paragraphs below describe these methods and offer a preliminary vision of how a program of analysis could unfold.
Vietnam, like other countries in rapid transition, does not commit enough resources to the fight against AIDS.[2] A comprehensive response to financing needs for HIV/AIDS will require just a quarter of one percent of GDP and a small share of total health spending in Vietnam (see Table 1). Resource mobilization is financially feasible but politically difficult.
Table 1: Prospective AIDS spending requirements, 5 CRT countries, spending per person, per PLHIV, as percentage of GDP and percentage of health spending, 2030/31
Full Coverage Spend, US$ millions |
AIDS Spend/ |
AIDS Spend/ |
AIDS Spend percent of GDP |
AIDS Spend percent Health Spend |
|
China |
$9,945 |
$6.68 |
$14,208 |
0.07 |
0.16 |
India |
$5,770 |
$4.07 |
$ 2,404 |
0.17 |
0.36 |
Indonesia |
$2,202 |
$7.71 |
$8,155 |
0.36 |
1.77 |
Thailand |
$328 |
$4.65 |
$538 |
0.09 |
0.26 |
Viet Nam |
$491 |
$4.62 |
$1,692 |
0.25 |
0.44 |
Source: Futures Institute projections of financing requirements under scenario of full coverage. AIDS spend/PLHIV assumes same number of PLHIV as estimated for 2007 in UNAIDS Report on the global AIDS epidemic 2008, Table 1, p. 219.
Money alone will not be enough to contain the epidemic. Politics (political will) and policy space could, in the years between now and 2031, matter more than money and fiscal space. Demonstrating the benefits of investing in prevention and harm reduction among IDUs, sex workers and MSM may help tilt the balance of political will in favor of these actions in Vietnam.
Harm reduction could be the cornerstone of a national program, implemented in several cases of Government-donor cooperation. To justify expanded Government commitment, future analysis needs to demonstrate and identify evidence of the returns on investment in HIV prevention. There are two major approaches now being employed in the health economics field:
- Calculation of program costs vs. the value of statistical lives saved and disability-adjusted life-years saved, employing approaches developed by W. Kip Viscusi, William Nordhaus, and David Cutler. A quick cost-benefit analysis (CBA) indicates that cost per IDU is about $80 annually. If, as with the Stover and others Science article, proposed targeted spending could prevent half the infections that they project would otherwise occur, a lives-saved approach can probably show a ratio of benefits to costs in the range of 5 to 8 and hence likely to be a sound investment;
- Cost-utility analysis that can demonstrate cost per infection averted by means of alternative combinations of prevention, care and treatment services, accompanied by estimation of costs saved as fewer persons ever becoming HIV+ lead to lower costs of ART and hence cost-savings from the interventions employed.
Each method has its advocates and uses; our objective must be to find results that can convince policy makers in Vietnam of the soundness of effective spending for HIV/AIDS interventions. Procedures and methods for these calculations could be developed in future stages of work on this topic.
ANNEX: Estimating the value of a statistical life
Health economists focus on the cost-effectiveness of health investments by estimating the cost per disability life-year (DALY) that can be saved with investments in prevention, care and treatment of a wide range of health services. Analysts using CBA will require that DALYs be translated into benefits in monetary terms. They can multiply DALYs by a country´s average per capita income expressed either at current exchange rates or by using common measures of purchasing power parity exchange rates expressed in international dollars. David Cutler pushed the benefits estimate even higher because GDP understates the value of additional lives; his analysis suggests that an additional year of life gained by health interventions is worth approximately 2.5 times the value of per capita income and product (Cutler 2004). Cost-benefit analysis (CBA) could consider the fuller range of non-health benefits that may derive from health improvements, e.g., greater productivity, more foreign direct investment, and increased international trade for private-sector producers;
Viscusi shows convincingly that a life saved in the USA is often compensated in the US legal system at a value of $3 million to $7 million. Cohen´s work shows that spending on HIV/AIDS interventions of an amount less than $250,000 per DALY saved is cost-effective, whereas Holtgrave, Pinkerton and their co-authors focus on $50,000 per DALY saved as a good buy in US health care services focusing on HIV/AIDS (Holtgrave and others, 1997, 2002, Pinkerton and others, 2000). These analyses, in both developed and less-developed country settings, demonstrated the potential gains from applying economic analysis in the health sector can be substantial.
David Cutler drew on the earlier work of Viscusi (1993), Viscusi and Aldy (2004), and Nordhaus (2002) to show that health interventions in the USA since 1960 brought far greater value in lives and life-years saved than they cost in terms of health spending. He shows, for example, that improvements in cardiovascular disease treatment alone saved more money and lives than the aggregated spending on all health care in the last half century.[3] In later work with Grant Miller, the authors calculated the life-saving benefits of extending water and waste sanitation capacity to the billions not now served and demonstrate via a counterfactual calculation that benefits would far exceed costs. (Cutler was the principal advisor to the Obama Administration during the run-up to passage of health reform legislation recently.)
By 2005, there was already broad though not universal agreement among health economists that lives and life-years saved are sound measures of benefits to be derived from health investments (Cf. Berman 1998. Their views are summarized in Priorities in health (Jamison and others 2006, and Disease control priorities (DCP2, ed., Jamison and others, 2006 and www.dcp2.org). Guidance provided there is also of direct utility for analysis of projects that the Vietnamese Government and its donors will consider.
Priorities in health, Chapter 3, sets out some key terms and their definitions summarized here:
- Units for cost-effectiveness ratios: Calculate cost-effectiveness in terms of US dollars per DALY (disability-adjusted life-year), where DALYs are calculated using disability weights provided by WHO and a 3 percent discount rate;
- No differentiation by age: Saving of an infant life counts for more than saving the life of an older person because of the difference in expected years of life; a year of life saved is equal at all ages;
- Basis for calculating years of life: Use regional life expectancy;
- Currency units: Convert local currencies to US dollars at current exchange rates or via International dollars at purchasing power parity;
- Costs: Count the costs of producing an intervention but not the costs of consuming it on the part of patients and their families (Jamison and others, 2006, 41).
Even without pricing a DALY, the analyst can calculate the cost per DALY gained. Comparisons with results emerging from CEA approaches would usefully complement and could potentially reassure health project analysts that a proposed project does or does not meet standard criteria for assessing health project investments. In summary:
- Cost-effectiveness analysis, basically the cost per DALY, would help promote a focus on the most cost-effective health sector interventions;
- Cost-benefit analysis (CBA) could consider the fuller range of non-health benefits that may derive from health improvements, e.g., greater productivity, more foreign direct investment, and increased international trade for private-sector producers;
- Vietnamese HIV/AIDS managers could weigh these risks along with its estimates of economic rate of return and the cost-effectiveness of health interventions in reaching its decisions.
Selected References
Aral, S.O. and M. Over, K.K. Holmes, L. Manhart, N. Padian, and S. Bertozzi. 2004. Sexually Transmitted Infections. Disease Control Priorities in Developing Countries 2005. Pre-publication.
Barnum, Howard. 2001. Economic evaluation of health projects. In Belli, P., and others, Economic analysis of investment operations. Analytical tools and practical applications. Pp. 99-119.
Becker, Gary. 1975. Human capital: A theoretical and empirical analysis with special reference to education. Chicago: University of Chicago Press, Second edition.
Belli, Pedro, Jock R. Anderson, Howard N. Barnum, John A. Dixon, and Jee-Peng Tan, editors. 2001. Economic analysis of investment operations. Analytical tools and practical applications. Wash DC: World Bank, WBI Development Studies. 264 p.
Bongaarts, John, and Mead Over. 2010. Global HIV/AIDS policy in transition. Science 328, 11 Jun 2010, 1359-60.
Centers for Disease Control. 1999. Ten great public health achievements — United States, 1900-1999, MMWR Morb Mortal Wkly Rep. 48:241-43.
Cohen, D.A. et al. 2004. Comparing cost-effectiveness of HIV prevention interventions. Journal of Acquired Immune Deficiency Syndrome 37: 1404-1414.
Cohen, D.A., S. Wu, and T. A. Farley. 2005. Cost-Effective Allocation of Government Funds to Prevent HIV Infection. Health Affairs. 24:4 p. 915-926.
Cutler, David. 2004. Your money or your life: Strong medicine for America´s healthcare system. New York: OUP.
Eckstein, Otto. 1958. Water resource development. The economics of project evaluation. Cambridge MA: Harvard University Press. 300 p.
Frederick, Shane, George Loewenstein, and Ted O´Donoghue. 2002. Time discounting and time preference, a critical review. Journal of economic literature XL, June, 351-401.
Gottret, Pablo, and George Schieber. 2006. Health financing revisited, a practitioner?ÇÖs guide. Wash DC: World Bank.
Gramlich, Edward. 1997. A Guide to Benefit-Cost Analysis. Second Ed. Waveland Press.
Jamison, Dean T, and others, Editors. 2006. Priorities in health. Wash DC: World Bank.
Nordhaus, William. 2002. The health of nations: The Contribution of Improved Health to Living Standards. Unpublished, NBER and Yale University Economics Department. 31 p.
Stover, J., and others. 2006. The global impact of scaling up HIV/AIDS prevention programs in low- and middle-income countries. ScienceExpress, 2 February and 10 March 2006.
Tan-Torres Edejer, T. et al (ed.). 2003. Making Choices in Health: WHO Guide to Cost-Effectiveness Analysis. Geneva: World Health Organization.
Tengs, T.O. and T. H. Lin. 2002. A Meta-Analysis of Utility Estimates for HIV/AIDS. Medical Decision Making. 22 p. 475-481.
Viscusi, W. Kip. 1993. The Value of Risks to Life and Health. Journal of Economic Literature 31, 4, 1912-1946.
Viscusi, W. Kip, and Joseph Aldy. 2003. The value of a statistical life: a critical review of market estimates throughout the world. The journal of risk and uncertainty 27, 1, 5-76.
World Bank. 1993. World development report: Investing in health. Wash DC: World Bank.
[1] Government of Vietnam: Fourth UNGASS report 2010
[2] No country in Asia meets the Independent Commission on Aids in Asia (ICAA) criterion of spending a half to a dollar per person per year on HIV/AIDS. Nor do these countries focus their efforts on the interventions that yield the greatest reductions in new infections and the most beneficial actions to extend lives and avoid premature deaths.
[3] See Cutler, David. 2004. Your money or your life: Strong medicine for America´s healthcare system. New York: OUP, pp. 47-75.
What is Happening with pre-ART Care in Sub-Saharan Africa?
June 13, 2011
What is happening with pre-ART care in sub-Saharan Africa?
Sydney Rosen
The remarkable expansion of access to antiretroviral therapy (ART) for HIV/AIDS in resource-constrained countries has given nearly four million HIV-positive adults in sub-Saharan Africa the opportunity to achieve what for many may be nearly normal life expectancies [1]. Others, however, do not make it past their first year on treatment. A major cause of the high rates of death and loss to follow up seen in most countries is late presentation for treatment [2]. Median starting CD4 counts have increased only modestly in the years since treatment became available [3,4], and most programs still report medians well below even the very low threshold of 200 cells/mm3 [5].
Earlier initiation of ART requires earlier diagnosis and regular monitoring until treatment eligibility. Poor pre-ART retention in care, or the failure to link patients from HIV testing to HIV care and retain them until they are eligible for ART, is a problem that has only recently begun to be recognized in the research literature. Without effective retention in pre-ART care, beginning with HIV testing and continuing until the first antiretrovirals (ARVs) are dispensed, even patients who have long been aware of their HIV status will access care only when seriously ill, which is often well after treatment eligibility.
Only a handful of quantitative studies reporting on rates of pre-ART linkage and loss in sub-Saharan Africa have been published, and many of these are limited in the time periods and outcomes they consider. A systematic review of the literature on patient retention between HIV testing and ART initiation in sub-Saharan Africa conducted in early 2011 [6] identified 24 papers and abstracts with quantitative data. As a way to synthesize this information, the pre-ART care period was divided into three stages, as illustrated in the figure below. Stage 1 lasts from a positive HIV test to receiving the results of an initial CD4 count (or clinical staging) and being referred to either pre-ART care or ART. Stage 2 is pre-ART care, spanning the period from enrollment in pre-ART until ART eligibility. Finally, Stage 3 lasts from ART eligibility to receipt of the first doses of ARVs. Patients can be lost (die, discontinue, or be lost to follow up) in any stage, as shown in the figure.
Figure: Stages of pre-ART care
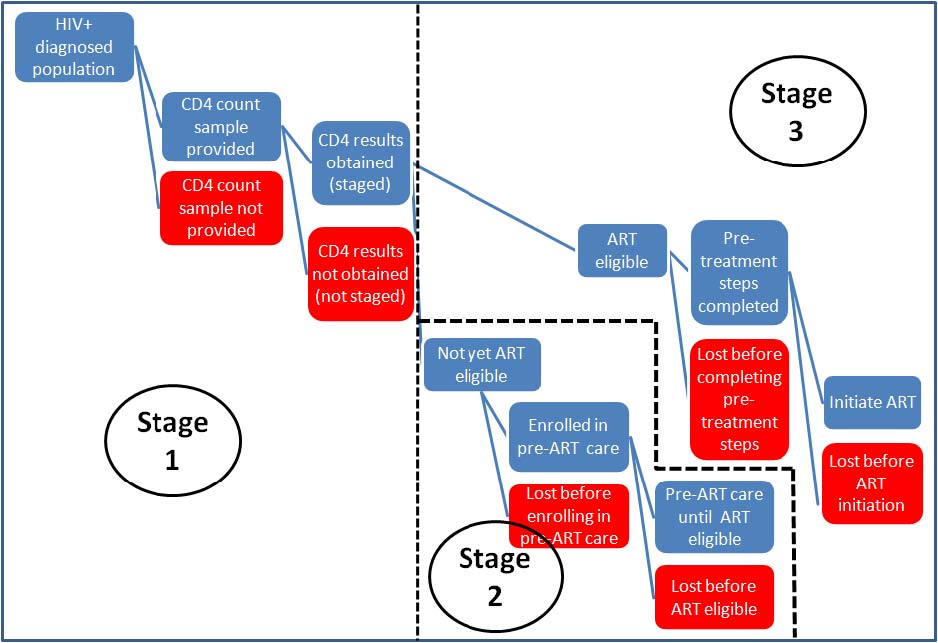
The literature review found that the median rates of retention (stage completion) for patients in sub-Saharan Africa were 52% in Stage 1, 46% in Stage 2, and 66% in Stage 3. Even with some optimistic assumptions about unreported losses, the review concluded that fewer than a third of all patients who test positive for HIV in this region and who are not yet eligible for ART remain continuously in pre-ART care until they reach eligibility. Pre-ART care, as it is currently structured, is thus failing to promote early initiation of treatment, and may be producing few benefits for the resources invested in it.
There appear to be several main reasons for the poor showing of pre-ART care. Most patients during this stage are asymptomatic and may not perceive themselves to require medical care. Since little therapeutic care is offered during the pre-ART period, patients must take on faith that making the effort to come to the clinic for monitoring is worth the costs of doing so. Current approaches to providing care often require multiple clinic visits, for example to first provide a blood sample for a CD4 count and then return a week later to receive the results. Choosing to "wait and see what happens" may well be a preferred strategy for patients who lack resources for transport, risk losing employment by taking time off work, or fear being recognized as a client of an HIV clinic. Other patients who present for care very late die before treatment can be initiated.
A number of interventions are being tried to improve retention in pre-ART care, though very few have been rigorously evaluated. Most interventions aim either to reduce the costs that patients perceive in seeking pre-ART care or increasing the perceived benefits of care. Interventions to reduce costs are more common and focus on structural changes in the delivery of care (fewer visits, more convenient locations, shorter waiting times, etc.). Interventions to increase benefits may offer more services at each visit (e.g. provision of cotrimoxazole or food parcels). There is little evidence so far as to whether these interventions will be effective, and no studies of cost-effectiveness were found.
The review identified two major obstacles to conducting quantitative research on pre-ART care. First, the terminology, definitions, time intervals, and outcomes used to describe and evaluate the pre-ART period are diverse and often poorly explained. Reaching a consensus on standard approaches and definitions would greatly improve the quality of current research. Second, there is an urgent need for health information systems that allow patients to be tracked between service delivery points. The review did not find a single study that was able to follow a cohort of HIV-positive adults all the way from testing to treatment initiation if they were not already eligible for ART when diagnosed. Researchers and program manager must implement effective patient tracking systems that will generate accurate information on the pre-ART period. Even doing this on a relatively small scale will be challenging, but it is vital for promoting early treatment initiation and improving resource allocation decisions.
References
1. WHO, UNAIDS, UNICEF. Towards universal access: Scaling up priority HIV/AIDS interventions in the health sector; Progress report 2010. Geneva: World Health Organization, 2010.
2. Brinkhof MW, Dabis F, Myer L, Bangsberg DR, Boulle A, Nash D et al.: Early loss of HIV-infected patients on potent antiretroviral therapy programmes in lower-income countries. Bull World Health Organ 2008, 86: 559-567.
3. Cornell M, Grimsrud A, Fairall L, Fox MP, van Cutsem G, Giddy J et al.: Temporal changes in programme outcomes among adult patients initiating antiretroviral therapy across South Africa, 2002-2007. AIDS 2010, 24: 2263-2270.
4. Keiser O, Anastos K, Schechter M, Balestre E, Myer L, Boulle A et al.: Antiretroviral therapy in resource-limited settings 1996 to 2006: patient characteristics, treatment regimens and monitoring in sub-Saharan Africa, Asia and Latin America. Trop Med Int Health 2008, 13: 870-879.
5. Fox MP, Rosen S: Patient retention in antiretroviral therapy programs up to three years on treatment in sub-Saharan Africa, 2007-2009: systematic review. Trop Med Int Health 2010, 15 Suppl 1: 1-15.
6. Rosen S, Fox MP. Retention in HIV care between testing and treatment in sub-Saharan Africa: a systematic review. Boston MA: Unpublished manuscript, Boston University Center for Global Health and Development, 2011.
Bringing HIV Programming Home: the Efficiency Possibilities of Country Ownership
June 16, 2011
Eileen Stillwaggon
Gettysburg College, Gettysburg PA, USA
Email: stillwaggon at gettysburg.edu
This IAEN series of papers is about effectiveness and efficiency of HIV/AIDS programming. Earlier contributions have made a persuasive case that effectiveness is context-specific, and that the pursuit of efficiency, too, may depend on who are the key players providing and allocating resources. Shrinking donations and country ownership could introduce some instability in the path of HIV prevention and treatment programs in low- and middle-income countries. But they also can stimulate a more aggressive search for efficiency in programming.
AIDS did not arise in isolation. The worst HIV epidemics are found in countries with multiple endemic diseases and inadequate health systems. In the early days of AIDS epidemics, national governments often raised the protest that their populations faced multiple health risks and the emphasis on HIV/AIDS was not proportionate to the burden of disease. While that approach was too conservative, given the enormity of the HIV epidemic, especially in southern Africa, it does point to some important opportunities for increased service delivery with greater efficiency.
Integrated health programs can enhance efficiency by taking advantage of economies of scale and of scope. They are also better suited to address diseases and other health problems, such as malnutrition, that have significant and multiple interactions. Vertical programs isolate funds for narrowly defined uses, missing the opportunities for positive externalities in health spending. Donor-driven programs tend to be vertical and reflect health priorities from the viewpoint of donors. Vertical programs make less sense with a shift in emphasis to country ownership, and that goes for HIV/AIDS as much as for any other health issue.
National ministries of health already address a wide range of health problems. There is the potential for better integration of diverse services when they are housed under one ?Çÿroof.´ With country ownership comes the opportunity to address the long-standing health problems of their populations with greater efficiency because of the possibilities for integrating multiple services that require similar facilities, equipment, and staff. HIV/AIDS programming can find a home in the ministry of health and in local clinics and hospitals, along with other pressing health concerns, many of which interact with HIV.
Integrating health services to improve efficiency has a biological evidence base, as well. Diseases can act synergistically, increasing susceptibility and contagiousness. Moreover, one of the ongoing problems with the AIDS pandemic is addressing co-infections, including TB, STIs, and hepatitis. Countries with good access to ART, such as Botswana, are finding that many women under treatment still die, but from cervical cancer. Comprehensive women´s and men´s health programs are needed to protect people living with HIV. Other co-infections endemic in tropical and sub-tropical poor populations also complicate both prevention and treatment.
Malaria increases HIV replication and viral load as much as ten-fold, doubling sexual and vertical transmission for several weeks after febrile episodes, which may recur several times in a year [1]. Moreover, treating malaria reduces HIV viral load [2]. Preventing HIV in malaria-endemic populations requires that we also prevent and treat malaria.
Another example of a common disease that interacts with HIV is urinary schistosomiasis, which affects almost 200 million people in sub-Saharan Africa. Women with genital lesions of schistosomiasis are three times as likely to be infected with HIV as women in the same villages without genital schistosomal lesions [3]. Treatment for schistosomiasis costs 7 US cents.
Effective treatment of HIV will also require an integrated approach. People infected with schistosomiasis often cannot tolerate antiretroviral therapy because a heavy parasite load impairs liver function. Moreover, trials have shown that CD4 counts can be increased in HIV-infected persons co-infected with ascaris (round worms) [4] by giving them deworming medication that costs about 2 US cents. It is likely that other intestinal helminthes have a similar impact on CD4 counts and viral load. Thus, it may be possible to postpone first-line antiretroviral therapy in these persons for a considerable length of time, protecting their health, increasing their productivity, and preserving first- and second-line therapies.
Just as TB treatment precedes ART, deworming should be part of the ART protocol. Trying to roll out ART without treating widespread, easily curable conditions like worms wastes lives and squanders first-line therapy. Deworming is safe, effective and easily dosed; it generates positive externalities (treating one person may reduce others´ risk of infection); and it might also prevent the failure of first-line ART ?Çô at a cost of as little as 2 US cents per person. The cost of moving to second-line therapy will far exceed the cost of treating coinfections. It is important to move as many people to early initiation of ART as possible. But we know that in poor populations many people will never have access to ART and many others will be sick too long before they start. If we can keep people healthy longer with simple, cheap treatment for highly endemic conditions, like worms, we will save more lives more efficiently. Even women who survive with ART treatment will die unless a more comprehensive protocol, like early screening for HPV and cervical cancer, becomes the standard.
It is possible to shift the entire distribution of risk of HIV acquisition and transmission in poor populations by focusing more on co-infections. When HIV/AIDS is isolated from other health concerns, that creates a bias against spending what are really trivial amounts to change the risk of transmission of HIV and the risk of treatment failure. Such investments are not a diversion of funds from HIV prevention and treatment; they are necessary complements. And they can best be implemented when HIV is part of a whole health approach.
Trying to solve one health problem at a time is doing things the hard (and expensive) way. It throws away the many opportunities to solve multiple problems simultaneously, and using lower-cost, higher-impact, readily available options.
Standard HIV-prevention policies, and thus cost-effectiveness analyses evaluating those interventions, have overlooked complementary investments for treating coinfections. Treatment for TB, schistosomiasis, malaria, malnutrition and helminthes is relatively inexpensive, highly effective, and essential for improving immune status in HIV-negative persons and decreasing viral load in HIV-infected persons.
To make a difference in the epidemic, it is not enough to accept programming as it is and try to deliver it more efficiently. Economists should be asking more fundamental questions about the causes of poor health in poor populations, including what is the constellation of factors in each country determining the spread of HIV there and leading to death following AIDS. The vast majority of HIV-prevention funding targets sexual behavior. Certainly sexual behavior influences individual risk, in any country. But the empirical evidence is clear that sexual behavior does not explain differences in population risk [5-8]. So far, cost-effectiveness studies of HIV-prevention interventions have generally produced Type III errors — they determine efficient solutions to the wrong problems.
It´s not much help to determine that an expensive campaign to change sexual behavior is cost-effective in changing sexual behavior (or maybe just effective in delivering the message, outcome unknown) if the larger reason that HIV spreads so rapidly in poor populations has little to do with sexual behavior. In that case, cost-effectiveness analysis gives us very precise, even correct answers to the wrong question.
Consequently, AIDS resources for prevention and treatment are squandered on the wrong prevention programs and on less effective treatment. With country ownership, ministries and NGOs need to own the right programs, and those programs will address broad health concerns of the population, including HIV. Effectiveness requires that HIV interventions address population risk, and that is a biological problem that derives from the health environment, not a behavioral problem. Efficiency requires that we stop chasing after one virus, one person at a time. We can do more with less, and we can do it better by focusing on health in integrated systems.
6. Stillwaggon, E. 2006. AIDS and the Ecology of Poverty. New York: Oxford University Press.



